It’s been months since seniors residing in nursing homes have seen their friends and family in person. The loneliness felt by all has been compounded by the vast amount of COVID-19 deaths in these facilities. Nursing home deaths from COVID-19 account for more than half of all fatalities in 14 states.
Between April 19 and May 8, more than 13,000 people living in long-term care facilities died from the virus, and at least one case of the virus has been reported in approximately one-third of nursing homes across the country.
How did this happen?
Long-term care facilities were hit hard for several reasons: highly concentrated populations of at-risk seniors who are more vulnerable to the virus, the delay in testing residents and the continued shortage of personal protective equipment (PPE). The culmination of these factors has made nursing homes the epicenter of COVID-19.
Could it also have been asymptomatic carriers that brought the virus into nursing facilities? Vince Mor, PhD, a Brown University researcher, believes that these carriers were largely responsible for the spread of COVID-19. After initially saying that people who didn’t show symptoms were unlikely to spread the coronavirus, the World Health Organization (WHO) has recently clarified their remarks saying that the actual rates of transmission aren’t yet known.
“The majority of transmission that we know about is that people who have symptoms transmit the virus to other people through infectious droplets,” Maria Van Kerkhove, the WHO’s technical lead on the pandemic, told STAT News. “But there are a subset of people who don’t develop symptoms and to truly understand how many people don’t have symptoms, we don’t actually have that answer yet.”
Citing nursing homes and related facilities as a “ground zero” of the crisis, Dr. Tom Frieden, the former head of the U.S. Centers for Disease Control and Prevention (CDC), called for visitors to be banned in early March. A few days later, federal authorities addressed the issue. On April 19, the Trump Administration required all nursing home cases to be reported to the CDC —later unveiling a COVID-19 case reporting tool and requirements.
Even more recently, the Centers for Medicare & Medicaid Services (CMS) has updated the Nursing Home Compare database to include individual building-level data on COVID-19 outbreaks. This database has been built from nursing home surveys that have been conducted since March 4.
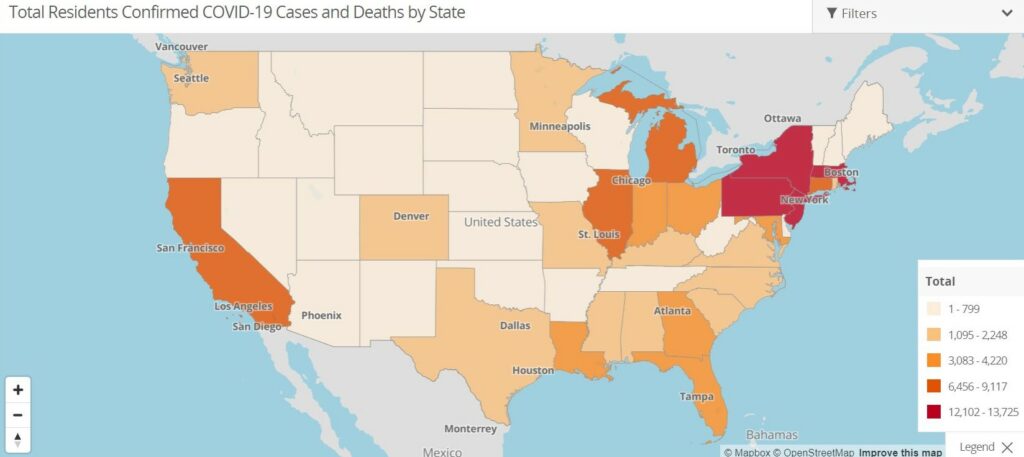
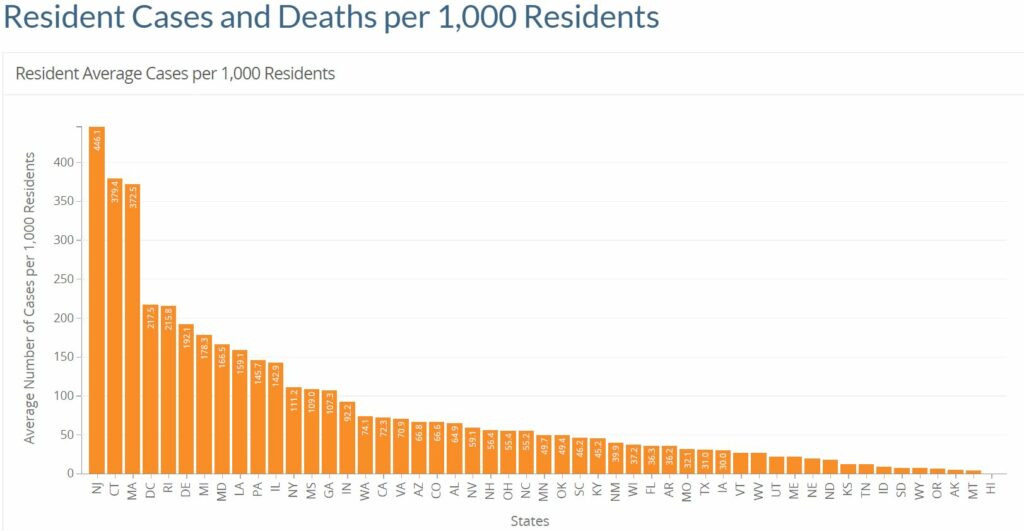
The website now includes an interactive map that provides a count of resident infections and deaths; aggregate data can be downloaded by researchers and reporters for further analysis. The data depicts higher COVID-19 numbers than previously reported by CMS — based on 88% of facilities reporting their data to the site. As of June 4, there has been nearly 32,000 COVID-19 deaths and more than 95,000 confirmed cases in long-term care facilities across the country.
Where we are now
On May 18, CMS released guidelines on reopening nursing homes. It emphasized that long-term care facilities should be the last to open in the country as the U.S. aims to lift lockdowns.
States can choose how they should implement the guidelines. Some highlights include:
- States can instruct facilities to reopen via regions or on a building-by-building basis.
- Nursing homes should test all residents and staff before going through the three phases of reopening.
- Staff will need to be screened daily and tested weekly.
- Nursing homes must report their monitoring and any COVID-19 cases to the CDC.
- Facilities with a significant outbreak must be inspected by state survey agencies prior to reopening.
Prior to CMS publishing the nursing home survey results, there had been public outcry about case reporting transparency. In Pennsylvania, families of seniors who needed long-term care demanded to know about facility-specific cases so they could safely place their loved ones. The reason for the uproar? About 70% of deaths from the virus were among residents in long-term care facilities in Pennsylvania.
The new face of nursing homes
How will COVID-19 impact nursing home operations and visits in the future? Some states have already begun taking measures and implementing operational changes as the nation slowly begins to reopen.
In Pennsylvania, regular staff and resident testing will be required, while a county in New York is testing every nursing home resident. This layer of testing may become the new normal as the latest CMS guidance has suggested similar testing across the country.
There is also the possibility that we see COVID-only facilities. Connecticut and Massachusetts are among a few states that have opened facilities that only accepts patients with the virus. Patients come directly from the hospital after treatment for coronavirus and also from other facilities that cannot segregate infected patients.
The pandemic has reinforced pushes for smarter facility design. Suggestions include nursing homes with more separation (i.e. individual living suites instead of rooms with multiple occupants). Nursing homes may also be equipped with better air filtration systems as well as ultraviolet light filters to kill airborne viruses.
Existing facilities could be updated with more easy-to-clean surfaces including antimicrobial materials such as copper. They may also see more voice- or motion-sensor controls for faucets, lighting, doors, etc.
Nursing homes must also have infection control plans and “would inherently need to inform staff about cases of COVID-19 in the facility” in order to enact them, an NBC News report said. Health and safety experts say that despite CDC recommendations, no one group is enforcing the measures or ensuring there are consequences.
Facilities will need a plan to protect their staff as well. Some nursing home advocates have been vocal about demanding better training and equipment to safeguard their employees. Without such protections and transparent reporting, the employees could retaliate, leaving gaps in care. The combination of new reporting requirements along with smarter rules aims to make it safer for workers to care for patients.
As for what it will look like when visitors are let back in, there are still a lot of questions. One of the major Opening Up America Again guidelines says that visitors shouldn’t be allowed unless there are no new cases at the facility for 28 days. But the plan doesn’t specifically address or mandate that workers be trained on how to use it effectively — something perhaps more common in hospitals but nevertheless just as vital in a nursing facility.
Life inside a nursing home over the past three months has been volatile, at best. The sheer number of senior lives lost is unforgettable and the impact on the surviving residents will be felt for years to come. The importance of choosing the right path forward is crucial to more than just your organization — it’s for your patients and their families, too.



